Implant
An orthopedic implant is a medical device manufactured to replace a missing joint or bone or to support a damaged bone. A dental implant is a material or device placed in and on oral tissue to support oral prostheses. A biomaterial is any substance that has been engineered to interact with biological systems for a medical purpose - either a therapeutic (treat, augment, repair or replace a tissue function of the body) or a diagnostic one. As a science, biomaterials are about fifty years old. The study of biomaterials is called biomaterials science or biomaterials engineering. It has experienced steady and strong growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
To replace a missing medical device many materials have been tried as an implant. With all the advancements and developments in the science and technology, the materials available for orthopaedic and dental implants also improved
The metallic biomaterials are conveniently grouped in the following items:
- Stainless steel
- Cobalt base alloys
- Titanium base alloys
- Specially metallic alloys
In the 1950s, stainless steel (18-8 Mo with very low carbon) was used for implant fabrication. This alloy has a very good resistance to chloride solutions and poor sensitization.
The castable CoCrMo alloy has been used for many decades in dentistry and, relatively recently, in making artificial joints. The wrought CoNiCrMo alloy is relatively new, now used for making the stems of prostheses for heavily loaded joints such as the knee and hip. Both alloys have excellent corrosion resistance.These alloys are characterized as following (table1):
Table 1
| Material designation | Common name ASTM |
| Stainless Steel | |
| Fe-18Cr-14Ni-2.5Mo | 316L Stainless Steel |
| Cobalt base alloys | |
| Co-28Cr-6Mo | Cast CoCrMo |
| Co-35Ni-20Cr-10Mo | Wrought CoNiCrMo |
Later, it was found that titanium was tolerated as was stainless steels and cobalt alloys. Titanium's lightness and good mechano-chemical properties are salient features for implant application. Titanium was found the only metal biomaterial to osseointegrate (Osseointegrated implant is a type of implant defined as "an endosteal implant containing pores into which osteoblasts and supporting connective tissue can migrate") Also, there were even assumptions on a possible bioactive behaviour due to the slow growth of hydrated titanium oxide on the surface of the titanium implant that leads to the incorporation of calcium and phosphorous.
Commercially pure titanium (Ti CP) and extra low interstitial Ti-6Al-4V (ELI) are the two most common titanium base implant biomaterials. These materials are classified as biologically inert biomaterials. As such, they remain essentially unchanged when implanted into human bodies. The human body is able to recognize these materials as foreign and tries to isolate them by encasing it in fibrous tissues. However, they do not promote any adverse reactions and are tolerated well by the human tissues. These metals do not induce allergic reactions such as has been observed with some stainless steels, which have induced nickel hypersensitivity in surrounding tissues.
Manufacturers use six different titanium-based biomaterials to fabricate implants. Each of these materials, including four grades of commercially pure titanium and two titanium alloys, has distinct mechanical and physical properties. Clinicians should recognize these differences for optimal treatment planning and patient care as following:
- Titanium base alloys
- Commercially pure Ti Ti CP (grade 1 to 4)
- Titanium alloys Ti-6Al-4V
Commercially pure titanium (Ti CP) and extra low interstitial Ti-6Al-4V are the two most common titanium base implant biomaterials. These materials are classified as biologically inert biomaterials. As such, they remain essentially unchanged when implanted into human bodies. The human body is able to recognize these materials as foreign and tries to isolate them by encasing it in fibrous tissues. However, they do not promote any adverse reactions and are tolerated well by the human tissues.
Commercially pure titanium (Ti CP) and Ti-6Al-4V have the following elements as impurities and micro alloys (table 2):
Table 2
| Element | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Ti6Al4V |
| N max | 0.03 | 0.03 | 0.05 | 0.05 | 0.5 |
| C max | 0.10 | 0.10 | 0.10 | 0.10 | 0.08 |
| H max | 0.015 | 0.015 | 0.015 | 0.015 | 0.0125 |
| Fe max | 0.20 | 0.30 | 0.30 | 0.50 | 0.25 |
| O max | 0.18 | 0.25 | 0.35 | 0.40 | 0.13 |
The mechanical properties of the Ti CP and the Ti6Al4V are given in Table 3.
Table 3
| Property | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Ti6Al4V |
| Tensile strength(MPa) | 240 | 345 | 450 | 550 | 860 |
| Yield strength (MPa) | 170 | 275 | 380 | 485 | 795 |
| Elongation(%) | 24 | 20 | 18 | 15 | 10 |
Corrosion Behavior of Metallic Bio-implant Alloys
The most common metallic biomaterials have high corrosion resistance. However, metallic biomaterials are not completely inert in the body. The presence of dissolved oxygen, chloride, phosphate, and organic molecules in the body fluids could influence their corrosion behavior. Protein is one of the components of the human body fluids. Body fluids contain different concentrations of protein and even the protein concentration varies at the implant/tissue interface during the healing period. Some proteins are negatively-charged at a neutral body pH and they react with the positively-charged ions released from metallic samples. The reactions either form an absorbed film on the surface of the samples or produce metal/protein/hydroxylated compounds.
Implant materials for orthopedic and heart surgical services demand a better corrosion resistance material than the presently used titanium alloys, where protective oxide layer breaks down on a prolonged stay in aqueous physiological human body, giving rise to localized corrosion of pitting, crevice, and fretting corrosion. A few surface treatments on Ti alloy, in the form of anodization, passivation, and thermal oxidation, followed by soaking in Hank solution have been found to be very effective in bringing down the corrosion rate as well as producing high corrosion resistance surface film as reflected from electrochemical polarization, cyclic polarization, and Electrochemically.
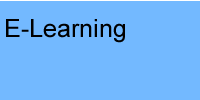
Orthopedic implant
An orthopedic implant is a device surgically placed into the body designed to restore function by replacing or reinforcing a damaged structure (fig 1), it means to replace a missing joint or bone or to support a damaged bon(fig 1). For the treatment of back pain, orthopedic implants such as bone plates and bone screws are used in spinal fusion surgery and fixation of fractured bone segments, as well as implant components used for hip and joint replacement. The material used in orthopedic implants must be biocompatible to avoid rejection by the body. The medical implant is mainly fabricated using stainless steel and titanium alloys for strength and the plastic coating that is done on it acts as an artificial cartilage. Other risks associated with orthopedic implants include implants coming loose or breaking in the bone causing painful inflammation and infection to surrounding tissue.
Orthopaedic implant technology is heavily based on the development and use of biomaterials. These are non-living materials (e.g. metals, polymers and ceramics) that are introduced into the human body as constituents of implants that fulfill or replace some important function.
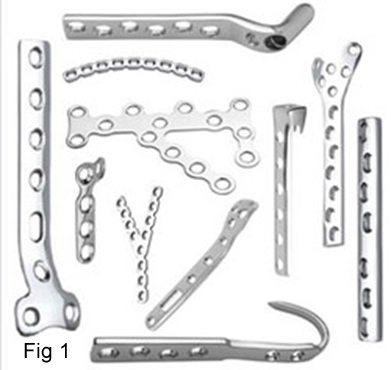
Dental implant
A dental implant is a material or device placed in and on oral tissue to support oral prostheses(fig 2).A dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biologic process called osseointegration where materials, such as titanium, form an intimate bond to bone. The implant fixture is first placed, so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic (a tooth, bridge or denture) is attached to the implant or an abutment is placed which will hold a dental prosthetic.
TYPES OF DENTAL IMPLANTS
There are four types of implant designs that have evolved during the centuries of development:
- Endosteal (in the bone): The first and most common type is ENDOSTEAL implants .The various types include screws, cylinders or blades surgically placed into the jawbone. Each implant holds one or more prosthetic teeth. This type of implant is generally used as an alternative for patients with bridges or removable dentures.
- Subperiosteal (on the bone): These are placed on top of the jaw with the metal framework's posts protruding through the gum to hold the prosthesis. These types of implants are used for patients who are unable to wear conventional dentures and who have minimal bone height.
- Transosteal implant combines the subperiosteal & endosteal components. This type penetrates both cortical plates & passes through full thickness of alveolar bone.
- Epithelial implant, which is inserted into the oral mucosa . Irrespective of implant design failure can occur due to local and systemic factors during replacement of missing teeth in surgical implant placement procedure.
Dental Implant Materials
Metals and Alloys (Titanium & Titanium –6 Aluminum-4Vanadium (Ti-6AI- 4V) and cp Ti, Cobalt-Chromium-Molybdenum-Based Alloy, Iron-Chromium-Nickel-Based Alloys), Ceramics (Aluminum, Titanium and Zirconium oxide, Bioactive and biodegradable ceramics) Carbon Carbon & carbon silicon, Vitreous and Pyrolytic) Polymers and Composites (Polymethylmethacrylate (PMMA), Polyethylene (UHMW-PE), Polytetrafluoroethylene (PTFE), Silicone rubber, Polysulfone).
Bone Augmentation Materials
CERAMICS (Calcium phosphate, Bioactive glass & glass ceramics), POLYMERS (PMMA, Lactic/glycolic acid), NATURAL MINERALS (Collagen, Demineralized bone matrix, Bone morphogenic proteins).